Antibiotics play a pivotal role in modern medicine, combating bacterial infections and saving countless lives. However, the world of antibiotics is diverse and complex, with various categories designed to target specific bacterial strains and mechanisms. In this comprehensive guide, we’ll delve into the diverse landscape of antibiotics, from beta-lactams to glycopeptides, exploring their mechanisms, uses, and importance in combating bacterial infections.
Introduction to Antibiotics
What are antibiotics?
Antibiotics are a class of medications that inhibit the growth of or destroy bacteria. They are crucial in treating bacterial infections, ranging from minor ailments to life-threatening conditions.
Importance of antibiotics in medicine
Since the discovery of penicillin by Alexander Fleming in 1928, antibiotics have revolutionized medicine, significantly reducing mortality rates from bacterial infections.
Evolution of antibiotic resistance
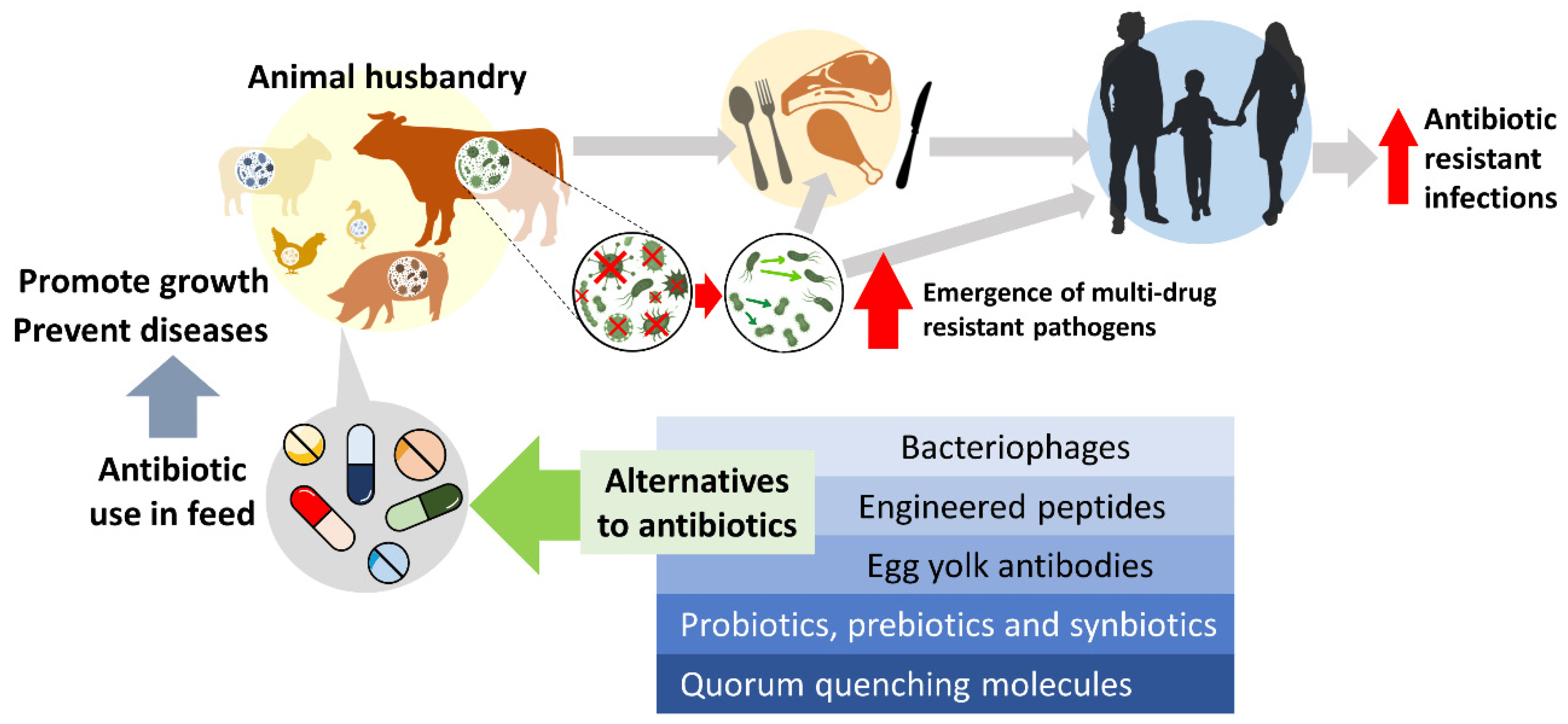
Despite their efficacy, overuse and misuse of antibiotics have led to the emergence of antibiotic-resistant bacteria, posing a significant global health threat.
Classification of Antibiotics
Antibiotics are classified based on their spectrum of activity and mechanism of action. Understanding these classifications is essential for selecting the appropriate antibiotic therapy.
Broad-spectrum vs. Narrow-spectrum antibiotics
Broad-spectrum antibiotics target a wide range of bacteria, while narrow-spectrum antibiotics are effective against specific bacterial strains.
Mechanism of action
Antibiotics exert their effects through various mechanisms, including inhibition of cell wall synthesis, protein synthesis, and nucleic acid synthesis.
Types of antibiotics based on structure
Antibiotics can be categorized into several classes based on their chemical structure, including beta-lactams, macrolides, quinolones, tetracyclines, sulfonamides, aminoglycosides, and glycopeptides.
Beta-lactam Antibiotics
Beta-lactam antibiotics are the most commonly prescribed class of antibiotics, comprising several subgroups:
Penicillins
Penicillins, such as amoxicillin and ampicillin, disrupt bacterial cell wall synthesis, leading to cell lysis and death.
Cephalosporins
Cephalosporins, like cephalexin and ceftriaxone, share a similar mechanism of action with penicillins but offer broader coverage against certain bacteria.
Carbapenems
Carbapenems, including imipenem and meropenem, are reserved for severe infections due to their broad spectrum of activity and potency.
Monobactams
Monobactams, such as aztreonam, are effective against Gram-negative bacteria and are often used in patients allergic to penicillins.
Macrolides
Macrolides are a class of antibiotics that inhibit bacterial protein synthesis. Common macrolides include:
Erythromycin
Erythromycin is effective against a wide range of bacteria and is commonly used to treat respiratory tract infections.
Clarithromycin
Clarithromycin is a second-generation macrolide with improved efficacy and fewer gastrointestinal side effects compared to erythromycin.
Azithromycin
Azithromycin is a broad-spectrum macrolide with a prolonged half-life, making it suitable for once-daily dosing.
Quinolones
Quinolones are synthetic antibiotics that interfere with bacterial DNA replication. They include:
Ciprofloxacin
Ciprofloxacin is commonly used to treat urinary tract infections and certain types of bacterial diarrhea.
Levofloxacin
Levofloxacin exhibits broad-spectrum activity and is often used to treat respiratory tract infections and skin infections.
Moxifloxacin
Moxifloxacin has enhanced activity against Gram-positive bacteria and is used in the treatment of respiratory and skin infections.
Tetracyclines
Tetracyclines inhibit bacterial protein synthesis and are effective against a wide range of bacteria. They include:
Doxycycline
Doxycycline is commonly used to treat acne, respiratory tract infections, and sexually transmitted diseases.
Minocycline
Minocycline is a second-generation tetracycline with improved penetration into tissues and broader spectrum of activity.
Tetracycline
Tetracycline is a broad-spectrum antibiotic used to treat various bacterial infections, including acne and urinary tract infections.
Sulfonamides
Sulfonamides inhibit bacterial folic acid synthesis and are used to treat urinary tract infections and other bacterial infections. Common sulfonamides include:
Sulfamethoxazole
Sulfamethoxazole is often combined with trimethoprim to form co-trimoxazole, a potent antibiotic combination used to treat a variety of infections.
Sulfadiazine
Sulfadiazine is used in the treatment of urinary tract infections and certain bacterial skin infections.
Aminoglycosides
Aminoglycosides inhibit bacterial protein synthesis and are particularly effective against Gram-negative bacteria. They include:
Gentamicin
Gentamicin is commonly used in combination with other antibiotics to treat severe bacterial infections, including sepsis and pneumonia.
Tobramycin
Tobramycin is often used to treat respiratory tract infections, particularly those caused by Pseudomonas aeruginosa.
Amikacin
Amikacin is a broad-spectrum aminoglycoside used to treat serious infections caused by multidrug-resistant bacteria.
Glycopeptides
Glycopeptides inhibit bacterial cell wall synthesis and are primarily used to treat Gram-positive bacterial infections. They include:
Vancomycin
Vancomycin is a potent antibiotic used to treat infections caused by methicillin-resistant Staphylococcus aureus (MRSA) and other resistant bacteria.
Teicoplanin
Teicoplanin is similar to vancomycin and is used in the treatment of serious Gram-positive infections.
Antibiotic Resistance
Antibiotic resistance has become a significant public health concern, driven by factors such as overuse, misuse, and inadequate infection control measures.
Causes of antibiotic resistance
Antibiotic resistance can arise due to genetic mutations, horizontal gene transfer, and selective pressure from antibiotic use.
Strategies to combat antibiotic resistance
Efforts to combat antibiotic resistance include antibiotic stewardship programs, infection prevention and control measures, and the development of new antibiotics and alternative therapies.
Side Effects and Precautions
While antibiotics are generally safe, they can cause side effects ranging from mild to severe. It’s essential to be aware of these side effects and take precautions when using antibiotics.
Common side effects of antibiotics
Common side effects of antibiotics include gastrointestinal disturbances, allergic reactions, and antibiotic-associated diarrhea.
Precautions while taking antibiotics
To minimize the risk of side effects and antibiotic resistance, it’s important to take antibiotics as prescribed, complete the full course of treatment, and avoid unnecessary antibiotic use.
Antibiotic Stewardship
Antibiotic stewardship aims to optimize antibiotic use to improve patient outcomes while minimizing the development of antibiotic resistance and reducing healthcare costs.
Importance of responsible antibiotic use
Responsible antibiotic use involves prescribing antibiotics only when necessary, selecting the appropriate antibiotic based on the type of infection, and optimizing dosing and duration of therapy.
Role of healthcare professionals in antibiotic stewardship
Healthcare professionals play a crucial role in antibiotic stewardship by promoting judicious antibiotic use, educating patients and colleagues about the risks of antibiotic resistance, and implementing evidence-based guidelines and policies.
Alternative Approaches to Antibiotics
In addition to traditional antibiotics, several alternative approaches show promise in combating bacterial infections.
Probiotics
Probiotics are live microorganisms that confer health benefits when consumed in adequate amounts. They have been studied for their potential role in preventing and treating certain bacterial infections.
Phage therapy
Phage therapy involves using bacteriophages, viruses that infect and kill bacteria, to treat bacterial infections. It shows promise as an alternative or adjunct to antibiotics, particularly in the era of antibiotic resistance.
Antibiotic peptides
Antibiotic peptides are naturally occurring molecules with antimicrobial properties. They offer a potential alternative to traditional antibiotics and are being investigated for their efficacy and safety.
Future of Antibiotics
The future of antibiotics is characterized by both challenges and opportunities.
Challenges and opportunities
Challenges include the rise of antibiotic-resistant bacteria, the decline in antibiotic discovery, and the need for innovative approaches to combat bacterial infections. However, opportunities exist in the form of new technologies, such as artificial intelligence and genomics, which may accelerate antibiotic discovery and development. Additionally, initiatives like Anabolics Canada are exploring novel strategies to address antibiotic resistance and promote the responsible use of antibiotics in healthcare settings.
Research and development in antibiotic discovery
Efforts are underway to identify novel antibiotics from natural sources, develop new antimicrobial agents, and explore alternative therapies, such as immunotherapies and phage therapy.
Conclusion
In conclusion, antibiotics are indispensable tools in modern medicine, offering effective treatment for bacterial infections. Understanding the diversity of antibiotic categories, their mechanisms of action, and the importance of responsible antibiotic use is essential for healthcare professionals and patients alike.
FAQs
What are antibiotics?
- Antibiotics are medications used to treat bacterial infections by either inhibiting the growth of bacteria or killing them.
What are the common side effects of antibiotics?
- Common side effects of antibiotics include gastrointestinal disturbances, allergic reactions, and antibiotic-associated diarrhea.
Why is antibiotic resistance a concern?
- Antibiotic resistance occurs when bacteria develop the ability to survive exposure to antibiotics, making infections harder to treat and increasing the risk of spread to others.
How can antibiotic resistance be prevented?
- Antibiotic resistance can be prevented by using antibiotics judiciously, completing the full course of treatment as prescribed, and implementing infection control measures.
What are alternative approaches to antibiotics?
- Alternative approaches to antibiotics include probiotics, phage therapy, and antibiotic peptides, which offer potential alternatives or adjuncts to traditional antibiotic therapy.